iTech has introduced a new feature called the expEDIum Direct Pay
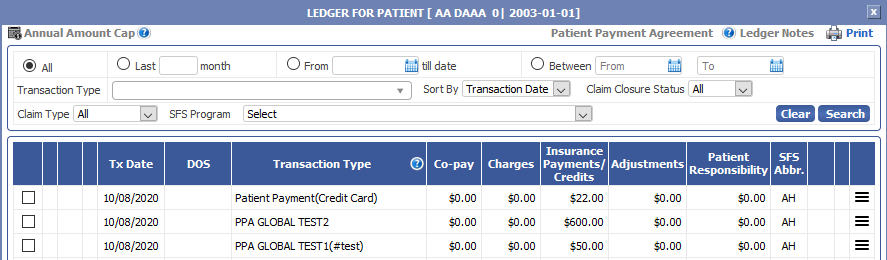
To do seamless online payments from Patient Ledger. The “expEDIum Pay” is a PCI-DSS certified standalone payment service application to route the online payment transactions for patients registered under a clinic/hospital in expEDIum Medical Billing through the chosen payment gateway.…